In the realm of reproductive health, advances in medical technology and surgical techniques have opened new doors for individuals and couples facing fertility challenges. Among these advancements, hysteroscopic surgery and tubal cannulation stand out as minimally invasive procedures with the potential to address specific causes of infertility related to the uterus and fallopian tubes. This blog delves into the nuances of these procedures, their indications, benefits, and what patients can expect during the treatment journey.
Understanding Hysteroscopic Surgery
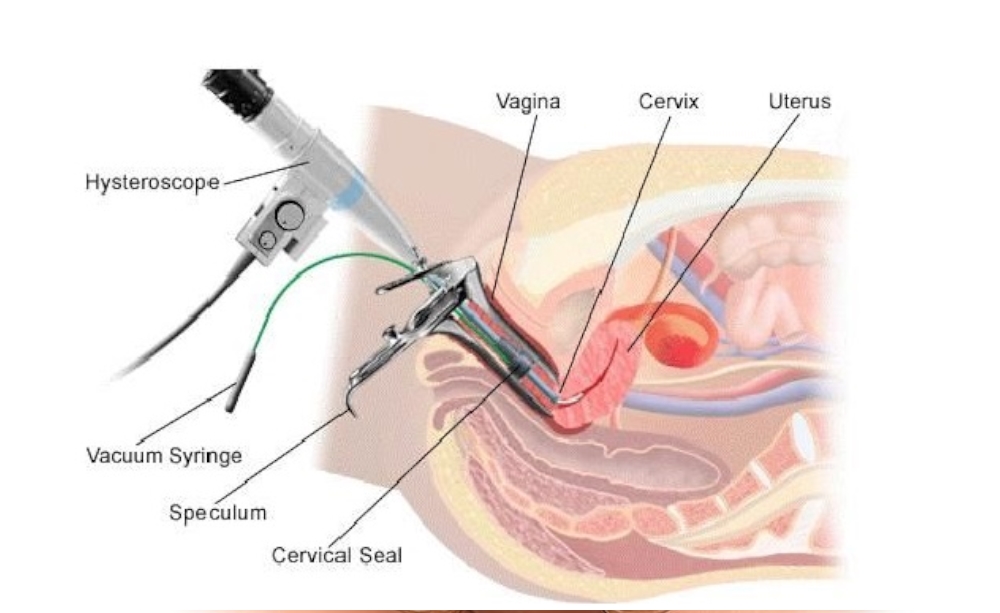
Hysteroscopic surgery is a minimally invasive procedure used to diagnose and treat uterine conditions without the need for abdominal incisions. The procedure involves the insertion of a hysteroscope, a thin, lighted telescope-like instrument, through the vagina and cervix into the uterus. This technique allows surgeons to visualize the inside of the uterus and perform surgical interventions if necessary.
Indications for Hysteroscopic Surgery
Hysteroscopic surgery can address various uterine conditions that may impact fertility, including:
- Removal of uterine fibroids or polyps
- Resection of uterine septa (a form of congenital uterine anomaly)
- Clearance of adhesions (scar tissue) within the uterine cavity
- Removal of retained products of conception following a miscarriage or incomplete abortion
Benefits of Hysteroscopic Surgery
The benefits of opting for hysteroscopic surgery include:
- Minimal invasiveness with no abdominal incisions
- Reduced recovery time compared to traditional open surgery
- Lower risk of infection and complications
- Improved chances of fertility by directly addressing uterine abnormalities
Exploring Tubal Cannulation
Tubal cannulation is a specialized procedure aimed at treating fallopian tube blockages, a common cause of female infertility. The procedure involves the use of a catheter, guided by a fluoroscope or hysteroscope, to clear blockages in the fallopian tubes, thereby restoring the pathway for eggs to travel from the ovaries to the uterus.
Indications for Tubal Cannulation
Tubal cannulation is primarily indicated for women with proximal tubal blockage, diagnosed through imaging tests such as a hysterosalpingogram (HSG). This procedure is particularly beneficial for those:
- With a diagnosed proximal tubal blockage
- Seeking to improve their chances of natural conception
- Looking for alternatives to more invasive fertility treatments like IVF
Benefits of Tubal Cannulation
- Non-surgical and minimally invasive approach
- Can often be performed on an outpatient basis
- Increases the possibility of natural conception
- Avoids the complexities and costs associated with assisted reproductive technologies (ART)
What Patients Can Expect
For those considering hysteroscopic surgery or tubal cannulation, understanding what to expect before, during, and after the procedure can ease anxieties and prepare one for the journey ahead.
Before the Procedure
- Comprehensive evaluation and diagnostic tests to determine the suitability for the procedure
- Discussion with the healthcare provider about the procedure details, potential risks, and success rates
During the Procedure
- Both procedures are typically performed under general anesthesia
- Duration varies from 30 minutes to a couple of hours depending on the complexity and specifics of the case
After the Procedure
- Recovery times are relatively short, with many patients returning to normal activities within a few days
- Follow-up appointments to monitor recovery and assess the success of the procedure in improving fertility
Conclusion
Hysteroscopic surgery and tubal cannulation represent significant advances in the field of reproductive medicine, offering hope and solutions to many facing the challenges of infertility. By addressing specific uterine and tubal issues, these minimally invasive procedures can enhance fertility outcomes, providing a less daunting path towards achieving pregnancy. As with any medical treatment, a thorough consultation with a fertility specialist is essential to determine the best approach based on individual health status and fertility goals.